Treatments For Disc Herniations
Treatment for herniated lumbar discs depends on the time and symptoms, anatomical/surgical considerations and the proper diagnosis.
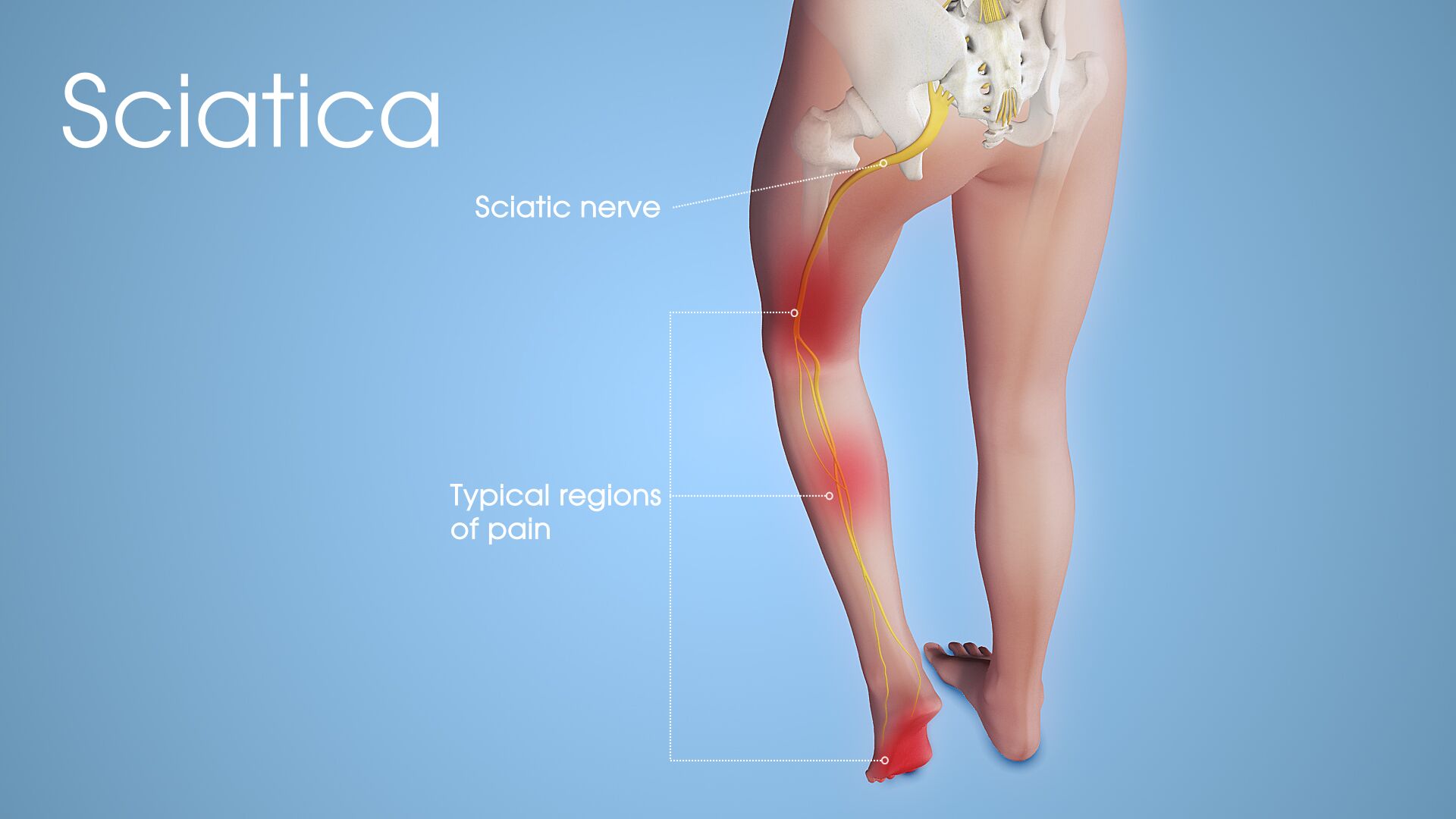
Proper Diagnosis: Complaints of back pain are very common and often resolve with little to no intervention. Many times patients come into the clinic with back pain and an MRI that shows a disk herniation, or at least says so on MRI report. Disc herniations classically cause sciatic pain down into the leg and foot with burning and numbness. But there is often a back pain component to the pain and there may be radiating pain into the leg that is not “classic” sciatic pain that extends below the knee. And there are times when disk herniations can cause just back pain with no leg pain component at all. Moreover, there are many patients that have an MRI that shows a disk herniation on films and report but have no symptoms of back or sciatic pain at all.
With that said, how do you treat a patient with back and leg pain with an MRI finding of a disk herniation? The first thing is to make the proper diagnosis with a good history and physical examination and independent review of the MRI’s by the spine doctor. There are essentially 5 things that typically cause back pain and the problem can be any or all of them or a combination of some and not others. Specifically they are:
- Muscular low back pain
- Facet pain (a series of small joints of the spine that allow bending and twisting)
- Sacroiliac joint pain
- Disk pain
- Hip pain
By a good examination, a spine doctor can separate out what is the main causes of the patient’s pain and suggest treatment. There is no substitute for a good history physical examination by a physician that knows what he or she is looking for. So from the standpoint of a spine doctor, the first thing to do when treating a disk herniation is making sure that it is really the main cause of the patient’s pain before you start treating it. From the standpoint of the patient, pick the right doctor.
Time Frame: Most back and sciatic pain improve with little to no treatment. Most often, improvement is seen in about 6 weeks. Patients are usually sent to physical therapy to prevent deconditioning of the back muscles while the underlying problem is healing. It is counterproductive to have a patient’s sciatic pain improve with time and end up with chronic back weakness.
Formal physical therapy, or alternatively home exercises, can help prevent chronic back weakness. In the first 6 weeks, patients can be treated with anti-inflammatory medications and a short course of muscle relaxants if there is back spasm. Narcotic medication is generally not indicated and should be avoided. Occasionally a short course of oral steroid medication is given for severe sciatic pain but that is not standard.
At 6 weeks, if there is no improvement the patient has likely already had an MRI and if not it should be ordered to confirm the presence of a disk herniation as the cause of the sciatic pain. At this point a lumbar epidural steroid injection should be considered to decrease pain and inflammation. An epidural steroid injection is generally more effective than oral steroids and longer lasting. It can be done by different techniques such as interlaminar or transforaminal. There are technical reasons why one would do one versus the other.
Click here to download a brochure on Lumbar Epidural Steroid Injections.
Contrary to popular belief, the epidural steroid injection does not heal the disk herniation. It decreases inflammation and pain so the patient can be more functional and do the low back exercises more effectively and get back to work sooner.
Generally, 1 or 2 epidural injections are all that is needed. Some physicians recommend a series of 3 injections or a series of a series of 3. Generally this is not necessary and delays appropriate treatment if the patient does not improve as quickly as expected.
In my opinion, only about 5% of patients with sciatic pain from a dick herniation need surgery. But if the sciatic pain persists at the 3 month period, despite non-surgical care, then it is time to consider surgery. The reason for this is that the results from surgery are best between the 3-6 month period. This is due to the fact that the nerves pressed by the disk herniation are not as likely to be chronically irritated and the back muscles have not been chronically deconditioned. This recommendation is supported in the literature and is also part of the formal recommendations of the North American Spine Society which I was fortunate to have been involved in writing. This is not to say that after 6 months that surgery is not effective. It is. But it is statistically more successful with shorter recovery and faster return to work if it is fixed between the 3-6 month period.
So bottom line is to get the patients in the hands of a qualified spine specialist early. Let the surgeon identify the 5% that will not improve with non-surgical care. And then fix the problem surgically within 6 months and the success rate approaches 95% with return excellent to normal life activities. Delay leads to more expense and greater likelihood of chronic pain with potential great economic expense and failure to return to life.
Anatomical/Surgical Considerations: There are many different ways to remove a symptomatic lumbar disc herniation. These include a laminectomy, a microdiscectomy and a lumbar endoscopic discectomy among others.
Click here to download our brochure on Laminectomy's Click here to download our brochure on Lumbar Endoscopic Discectomy
Bottom line is, they all work well and have excellent results. The difference is what needs to be done surgically to treat the problem at hand and how quickly the patient will recover.
From the standpoint of recovery, the smaller the incision and the less muscle dissection done in order to remove the disk herniation the faster the patient will recover.
Sometimes, the smaller incision will not address the entire problem and an open procedure, such as a laminectomy, is needed. This would be in a situation where there are many bony spurs that need to be removed along with the disk herniation in order to take full pressure off the nerves. A smaller procedure may have less muscle dissection and quicker muscle recovery but if the underlying problem is not fixed the patient will not improve and you have not accomplished your goal of getting the patient better and back to work.
Generally, you should choose the smallest procedure with the least dissection that will get the job done. And you should pick a surgeon that is familiar with all techniques so the right one can be chosen. Do not pick a surgeon that cannot do a variety of procedures (Read: How to Choose a Spine Surgeon). A Fellowship Trained Spine Surgeon Board Certified in Orthopedic Surgery or Neurosurgery is the best choice. They are trained in all the techniques and can pick what is best for the patient.
