Cervical VS. Lumbar Disc Herniation
What are the differences between a cervical and lumbar disc herniation in terms of symptoms, treatment and recovery?
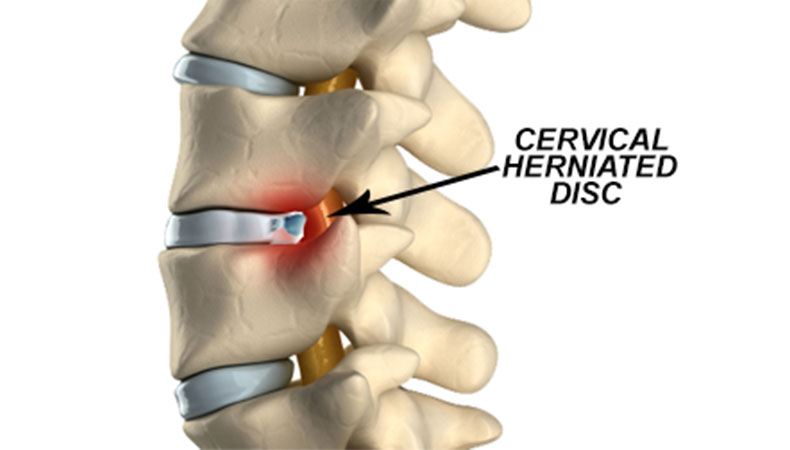
Cervical disk herniations are in the neck and lumbar disk herniations are in the low back. Because of this anatomic basic fact, there is one major difference between cervical and lumbar disk herniations to consider from the start.
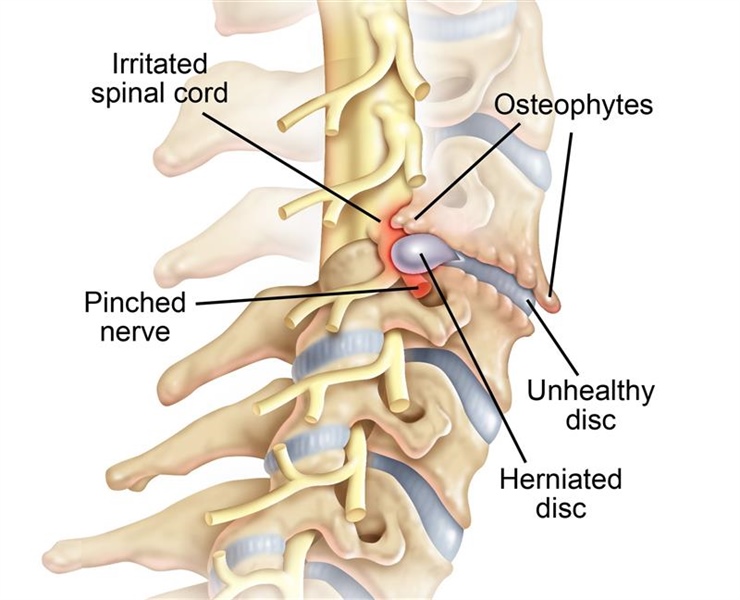
In the neck, there is the spinal cord and in the very low back where most herniations occur there are only nerve roots and no spinal cord. In the cervical spine, the nerve roots come off the spinal cord and go into the arms. Because of this, a cervical disk herniation can compress either the spinal cord or nerve roots or both. Nerve root compression alone from a disk herniation in the neck can cause typical arm pain and numbness and sometimes weakness. With the exception of significant arm weakness, these symptoms can often be treated non-surgically. Spinal cord compression from a cervical disk herniation, on the other hand, is different and can cause paralysis in both the arms and legs. We refer to this type of paralysis as “myelopathy”. The types of symptoms of myelopathy are a serious and often require surgery.
In contrast, in the very the low back, there is no spinal cord. As in the neck, a lumbar disk herniation can compress a nerve root but, in this case, the symptoms would be: Leg pain, Numbness or Weakness. With the exception of progressive weakness, the symptoms of a lumbar disk herniation can also often be treated non-surgically. Of note, a higher lumbar disk herniation at T12-L1 can injure many nerve roots at the same time, producing a surgical emergency called “cauda equina”. This is not common. Lumbar disk herniations are typically in the lower lumbar spine. When they are on occasion in the upper lumbar spine, they usually are not associated with cauda equina.
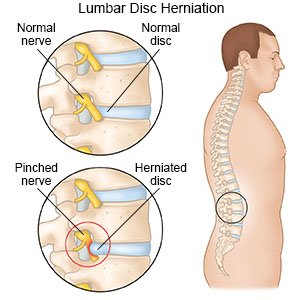
Lumbar Disc Herniation: Surgery & Recovery
With the exception of myelopathy or progressive weakness, both cervical and lumbar disk herniations symptoms usually resolve with non-surgical care including physical therapy and occasionally injections, such as epidural steroid injections. Learn more about Lumbar Disc Herniation here!
The surgical treatment of cervical and lumbar disk herniation is also somewhat different and it relates to the anatomy. Lumbar disk herniations with typical sciatic pain are treated almost without exception from the posterior approach. This posterior approach can be midline or off to the side and it can be done open or with a small endoscope. It is not typically done from the front of the body and the spine is typically not fused. The reason is that a typical lumbar disk herniation is compressing a nerve root producing leg symptoms of pain. The herniation is in the posterior aspect of the disk so the posterior approach is preferred. Even with large lumbar disk herniations, most of the disk is still intact and removing any more disk than the disk herniation itself is usually not necessary. As mentioned, there are different ways to remove a lumbar disk herniation from the posterior approach.
The time frame for recovery of a cervical versus a lumbar disk herniation is a bit different and somewhat more controversial. For lumbar disk herniations, there usually is improvement in symptoms between the 6 week to 3 month period. If there is no symptom relief despite non-surgical care during this time frame, then surgical intervention can be considered. If surgical intervention for a lumbar disk herniation is being considered, it has the greatest chance of success between the 3–6 month period. Relief of pain from surgery during this time frame approaches 95%. After 6 months the chance of pain relief is still very good but is falls below the 95% range. The reasons for this are not completely clear but probably has to do with chronic nerve irritation that becomes more likely permanent irritation after 6 months.
Note: Numbness and weakness in the legs from a lumbar disk herniation is more resistant to surgical treatment and is more likely to persist after surgical removal of a disk herniation.
Cervical Disc Herniation: Surgery & Recovery
Cervical disk herniations are in my opinion a bit different. I will usually give the symptoms 6 months to resolve before I will consider surgical intervention in most cases. This is my expert surgical opinion as I have seen many cervical disk herniation symptoms improve close to the 6-month period with non-surgical care. Other surgeons may differ on this point. Learn more about Cervical Disc Herniation here!
Posterior Approach
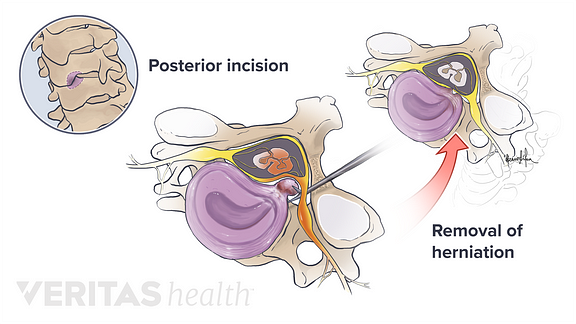
Cervical disk herniations are a bit different than lumbar herniations and are treated with varying techniques. As with the lumbar disk herniations, the symptomatic cervical disk herniation itself is posterior. But the posterior approach to the cervical spine is much more controversial. The spinal cord is in the posterior aspect of the neck and the posterior approach risks injury to the spinal cord. Not common but certainly a risk. There are smaller endoscopic techniques that use small incisions from the back of the neck that can be used to minimize risk. Larger disk herniations in the neck are harder to remove posteriorly because of the proximity of the spinal cord and the posterior approach may not be the best option. Much of it depends on the surgeons experience concerning which cervical disk herniations can be treated by the posterior approach and how best to minimize risk to the spinal cord. One problem for all posterior approaches is that the posterior approach does not address problems with the disk itself. In a cervical disk herniation, there is often injury to the entire disk. This is because the size of the disk in the neck is so small and a herniation affects a significant percentage of the disk structure. In the low back, the disk is large and a herniation there usually does not affect the entire disk. In a large cervical disk herniation, one may see some element of disk collapse or narrowing because of the herniation itself affects the structural support of the entire disk. This may not be apparent initially but develop over time as the disk structure slowly falls apart. These types of problems are not addressed by the posterior approach that only removes the disk herniation.
Anterior Approach

The anterior approach does address these structural issues but not without some tradeoffs. Going from the front to get to a disk herniation in the posterior aspect of the disk requires going through the body of the disk itself and removing a significant portion of the disk in the process of getting to the actual disk herniation. The resulting empty space needs to be filled in so as not to lead to further structural collapse and subsequent neck pain of worse. Options to fill up the empty disk space are with a cage or bone or both. This would be what is known as cervical fusion. Instrumentation is also typically used with a cervical fusion. This instrumentation can be a plate or cage with screws. Although the success for relieving pain from a cervical fusion approach is 95%, there are downsides. A cervical fusion may lead to degeneration of the remaining disks in the neck as they are making up for the lost motion at the fused levels and can wear out faster.
To prevent this subsequent disk degeneration at other levels surrounding the cervical fusion, other options have been developed. A cervical disk replacement can be considered. A cervical disk replacement attempts to replicate the normal motion of the cervical disk and prevent other disks around it from wearing out faster. And it probably does do that. Therfore, a cervical disk replacement is another option to treat a symptomatic cervical disk herniation form the front. But not everyone can be treated with a cervical disk replacement. From a technical standpoint, there cannot be a lot of arthritis at the surgical level of the disk herniation. Essentially, the disk replacement implant won’t fit in the disk space. Fortunately, a skilled spine surgeon can make the appropriate decision with the patient.
I should mention that an anterior cervical endoscopic discectomy can also be done in instances when the disk herniation is smaller and there is less risk of subsequent disk collapse. The surgical treatments of a cervical disk herniation are in general more varied than the surgical treatment of a lumbar disk herniation because of the size of the disk and the presence of the spinal cord near the herniation.
In summary, there are similarities and differences in treating symptomatic disk herniations in the neck and back. I tell my patients that the neck and back are different animals – similar but different. And as such, they are treated differently by a skilled surgeon depending on the patient’s symptoms and needs.
